Heel Pain And Discomfort
Overview
The most common form of Heel Pain, is pain on the bottom of the heel. It tends to occur for no apparent reason and is often worse when first placing weight on the foot. Patients often complain of pain the first thing in the morning or after getting up to stand after sitting. The pain can be a sharp, searing pain or present as a tearing feeling in the bottom of the heel. As the condition progresses there may be a throbbing pain after getting off your feet or there may be soreness that radiates up the back of the leg. Pain may also radiate into the arch of the foot.
Causes
A sharp stabbing pain, like a nail going into the bottom of the heel when first stepping on the foot after getting out of bed or after sitting for period of time, is the most common description for plantar fasciitis or heel spur syndrome. Typically the pain eases off as the day goes on but it may not go away completely. A thick ligament that attaches to the bottom of the heel and runs the length of the foot to the toes can become inflamed and swollen at the attachment site. This tends to be an overuse type of injury where poor foot structure is involved; also, wearing of shoe gear that lacks adequate support (ie: worn out shoes, boots and flip-flops) and prolonged standing or walking are often implicated. A throbbing pain that gets worse as the day goes on and can be worse at night when laying in bed is most often associated with an irritated or entrapped nerve on the inside of the ankle or heel. This is similar to carpel tunnel syndrome in the wrist and hand. Approximately 7 / 10 patients with heel pain have a component of nerve entrapment as the cause of their heel pain. This is also one of the most common causes of chronic heel pain because it is often missed as a diagnosis. When nerve entrapment is considered to be a cause, painless neurosensory testing is performed with the Pressure Specified Sensory Device? (PSSD) at The Foot & Ankle Center, PC to determine the extent of compression. A less common cause of heel pain but a stress fracture is often considered in athletes, such as long distance runners, who have heel pain. Posterior Heel Pain (Retrocalcaneal) This is pain in the back of the heel that flares up when first starting an activity. It is often associated with a large bump that can be irritated by shoes. The Achilles tendon attaches to the back of the heel and, like on the bottom, this attachment site can often become inflamed; a spur may or may not be present. Another painful area is a sac of fluid (bursa) that sits between the tendon and bone to act as a cushion for the tendon. This bursa can become inflamed often leading to significant pain called retrocalcaneal bursitis.
Symptoms
The heel can be painful in many different ways, depending on the cause. Plantar fasciitis commonly causes intense heel pain along the bottom of the foot during the first few steps after getting out of bed in the morning. This heel pain often goes away once you start to walk around, but it may return in the late afternoon or evening. Although X-ray evidence suggests that about 10% of the general population has heels spurs, many of these people do not have any symptoms. In others, heel spurs cause pain and tenderness on the undersurface of the heel that worsen over several months. In a child, this condition causes pain and tenderness at the lower back portion of the heel. The affected heel is often sore to the touch but not obviously swollen. Bursitis involving the heel causes pain in the middle of the undersurface of the heel that worsens with prolonged standing and pain at the back of the heel that worsens if you bend your foot up or down. Pump bump, this condition causes a painful enlargement at the back of the heel, especially when wearing shoes that press against the back of the heel. Heel bruises, like bruises elsewhere in the body, may cause pain, mild swelling, soreness and a black-and-blue discoloration of the skin. Achilles tendonitis, this condition causes pain at the back of the heel where the Achilles tendon attaches to the heel. The pain typically becomes worse if you exercise or play sports, and it often is followed by soreness, stiffness and mild swelling. A trapped nerve can cause pain, numbness or tingling almost anywhere at the back, inside or undersurface of the heel. In addition, there are often other symptoms, such as swelling or discoloration - if the trapped nerve was caused by a sprain, fracture or other injury.
Diagnosis
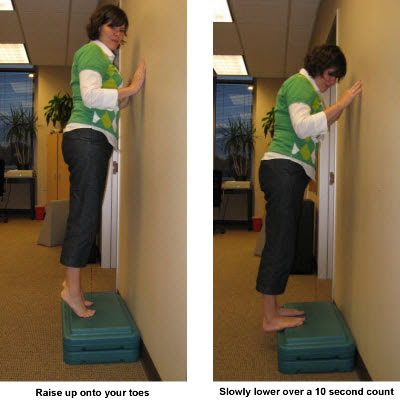
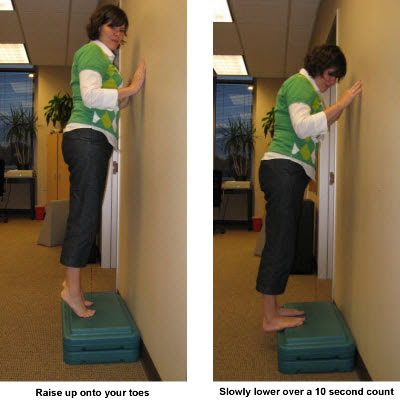
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
There are many treatments for fasciitis. The most common initial treatment provided by the family doctor are anti-inflammatory medications. They may take the edge off the pain, but they don't often resolve the condition fully. Steroid injections, which deliver the medication directly to the most painful area, are usually more effective. Rest, ice, weight loss, taping, strapping, immobilization, physiotherapy, massage, stretching, heel cushions, acupuncture, night splints and extra-corporeal shock wave therapy all help some patients. Many patients, however, have a biomechanical cause such as excessively pronated feet to their complaint, and this may mean many of the treatments listed above will only provide temporary relief of fasciitis symptoms. When you stop the treatment, the pain often returns. This is why many cases of fasciitis respond well to orthoses, custom-made inserts that control the mechanical cause of the complaint. If you're considering orthoses, it's very important to have a podiatrist specializing in the field to examine you. There are many biomechanical factors to consider when assessing the need for literally dozens of types of devices available, so you need to have an expert to properly assess you. (Unfortunately, as is the case in many jurisdictions, there is no minimum standard of training required in British Columbia to make orthoses, and there are many fly-by-night operations around that employ salesmen with little, if any, training in understanding anatomy or foot function. The emphasis with these groups is on selling you some sort of device, rather than providing proper assessment, treatment and follow-up.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
Prevention

Wear shoes that fit well, front, back and sides and have shock-absorbent soles, rigid uppers and supportive heel counters. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm-up before running or walking, and do some stretching exercises afterward. Pace yourself when you participate in athletic activities. If overweight, try non weight-bearing activities such as swimming or cycling. Your podiatrist may also use taping or strapping to provide extra support for your foot. Orthoses (shoe inserts) specifically made to suit your needs may be also be prescribed.
The most common form of Heel Pain, is pain on the bottom of the heel. It tends to occur for no apparent reason and is often worse when first placing weight on the foot. Patients often complain of pain the first thing in the morning or after getting up to stand after sitting. The pain can be a sharp, searing pain or present as a tearing feeling in the bottom of the heel. As the condition progresses there may be a throbbing pain after getting off your feet or there may be soreness that radiates up the back of the leg. Pain may also radiate into the arch of the foot.
Causes
A sharp stabbing pain, like a nail going into the bottom of the heel when first stepping on the foot after getting out of bed or after sitting for period of time, is the most common description for plantar fasciitis or heel spur syndrome. Typically the pain eases off as the day goes on but it may not go away completely. A thick ligament that attaches to the bottom of the heel and runs the length of the foot to the toes can become inflamed and swollen at the attachment site. This tends to be an overuse type of injury where poor foot structure is involved; also, wearing of shoe gear that lacks adequate support (ie: worn out shoes, boots and flip-flops) and prolonged standing or walking are often implicated. A throbbing pain that gets worse as the day goes on and can be worse at night when laying in bed is most often associated with an irritated or entrapped nerve on the inside of the ankle or heel. This is similar to carpel tunnel syndrome in the wrist and hand. Approximately 7 / 10 patients with heel pain have a component of nerve entrapment as the cause of their heel pain. This is also one of the most common causes of chronic heel pain because it is often missed as a diagnosis. When nerve entrapment is considered to be a cause, painless neurosensory testing is performed with the Pressure Specified Sensory Device? (PSSD) at The Foot & Ankle Center, PC to determine the extent of compression. A less common cause of heel pain but a stress fracture is often considered in athletes, such as long distance runners, who have heel pain. Posterior Heel Pain (Retrocalcaneal) This is pain in the back of the heel that flares up when first starting an activity. It is often associated with a large bump that can be irritated by shoes. The Achilles tendon attaches to the back of the heel and, like on the bottom, this attachment site can often become inflamed; a spur may or may not be present. Another painful area is a sac of fluid (bursa) that sits between the tendon and bone to act as a cushion for the tendon. This bursa can become inflamed often leading to significant pain called retrocalcaneal bursitis.
Symptoms
The heel can be painful in many different ways, depending on the cause. Plantar fasciitis commonly causes intense heel pain along the bottom of the foot during the first few steps after getting out of bed in the morning. This heel pain often goes away once you start to walk around, but it may return in the late afternoon or evening. Although X-ray evidence suggests that about 10% of the general population has heels spurs, many of these people do not have any symptoms. In others, heel spurs cause pain and tenderness on the undersurface of the heel that worsen over several months. In a child, this condition causes pain and tenderness at the lower back portion of the heel. The affected heel is often sore to the touch but not obviously swollen. Bursitis involving the heel causes pain in the middle of the undersurface of the heel that worsens with prolonged standing and pain at the back of the heel that worsens if you bend your foot up or down. Pump bump, this condition causes a painful enlargement at the back of the heel, especially when wearing shoes that press against the back of the heel. Heel bruises, like bruises elsewhere in the body, may cause pain, mild swelling, soreness and a black-and-blue discoloration of the skin. Achilles tendonitis, this condition causes pain at the back of the heel where the Achilles tendon attaches to the heel. The pain typically becomes worse if you exercise or play sports, and it often is followed by soreness, stiffness and mild swelling. A trapped nerve can cause pain, numbness or tingling almost anywhere at the back, inside or undersurface of the heel. In addition, there are often other symptoms, such as swelling or discoloration - if the trapped nerve was caused by a sprain, fracture or other injury.
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
There are many treatments for fasciitis. The most common initial treatment provided by the family doctor are anti-inflammatory medications. They may take the edge off the pain, but they don't often resolve the condition fully. Steroid injections, which deliver the medication directly to the most painful area, are usually more effective. Rest, ice, weight loss, taping, strapping, immobilization, physiotherapy, massage, stretching, heel cushions, acupuncture, night splints and extra-corporeal shock wave therapy all help some patients. Many patients, however, have a biomechanical cause such as excessively pronated feet to their complaint, and this may mean many of the treatments listed above will only provide temporary relief of fasciitis symptoms. When you stop the treatment, the pain often returns. This is why many cases of fasciitis respond well to orthoses, custom-made inserts that control the mechanical cause of the complaint. If you're considering orthoses, it's very important to have a podiatrist specializing in the field to examine you. There are many biomechanical factors to consider when assessing the need for literally dozens of types of devices available, so you need to have an expert to properly assess you. (Unfortunately, as is the case in many jurisdictions, there is no minimum standard of training required in British Columbia to make orthoses, and there are many fly-by-night operations around that employ salesmen with little, if any, training in understanding anatomy or foot function. The emphasis with these groups is on selling you some sort of device, rather than providing proper assessment, treatment and follow-up.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
Prevention

Wear shoes that fit well, front, back and sides and have shock-absorbent soles, rigid uppers and supportive heel counters. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm-up before running or walking, and do some stretching exercises afterward. Pace yourself when you participate in athletic activities. If overweight, try non weight-bearing activities such as swimming or cycling. Your podiatrist may also use taping or strapping to provide extra support for your foot. Orthoses (shoe inserts) specifically made to suit your needs may be also be prescribed.